Skin Engineering
Tissue and Knowledge Grow in SIU's Regenerative Medicine Lab
By Steve Sandstrom | Illustration by Lauren Woldanski, MD
Within an operating room, surgeons sometimes notice little things that they wish they could do better. A change that could improve the medical outcome or the patient’s post-op convalescence is not to be ignored.
For Michael Neumeister, MD, professor and endowed chair of SIU’s Department of Surgery, a recurring concern involved “borrowing.” Removing healthy tissue from one site on the anatomy to fix another is common practice in reconstructive surgery. It helps a patient’s recovery from a body trauma caused by cancer, an accident or a congenital abnormality. For instance, Dr. Neumeister would take bone and skin from a person’s leg to fix a missing section of the jaw.
As appreciative as his patients were for the repairs he had made, he knew this was causing them a new, secondary source of discomfort. Dr. Neumeister began investigating what was scientifically possible to minimize the use of these donor sites.
The process of tissue engineering had gained popularity in the ‘90s, and Dr. Neumeister made it his research focus.
“I thought, what if I could restore form and function with something created in the lab, or even better, within your own body, by allowing the fluids and growth proteins that we all have to make a scar matrix or a trachea by modifying the environment in say, the leg, to create something that we can then move up to the neck,” he says.
Twenty-five years later, what was once theory is now closer to practice. Dr. Neumeister directs research projects to build back better in SIU’s Regenerative Medicine and Microsurgical Education Laboratory. The lab’s innovations include developing hair-bearing skin using hair follicle stem cells; modifying fat to form nerve, cartilage and bone; ear and trachea reconstruction; and actual bone reconstruction.
Lab manager Carrie Harrison, researcher Michelle Randle and a team of young resident physicians are working with Neumeister to take the next steps to advance tissue engineering, and resolve the scarring left from borrowing. The translational goal is to bring this type of basic science research out of the lab and into the O.R. and clinics as quickly and safely as possible.
The corps of residents provide more than labor at the bench. Dr. Neumeister sees it as a way to invigorate the science. “I encourage them to have their own ideas, come to me with questions and together we’ll try to solve them and find the right answers.” They collaborate on grant proposals to generate funding or Neumeister will see if internal funds are available.
The surgical chair is comfortable complementing work in both clinical and basic science research. “Not everyone has an aptitude for basic science, but every one of the residents is inquisitive,” he says.
BODY REBUILDERS
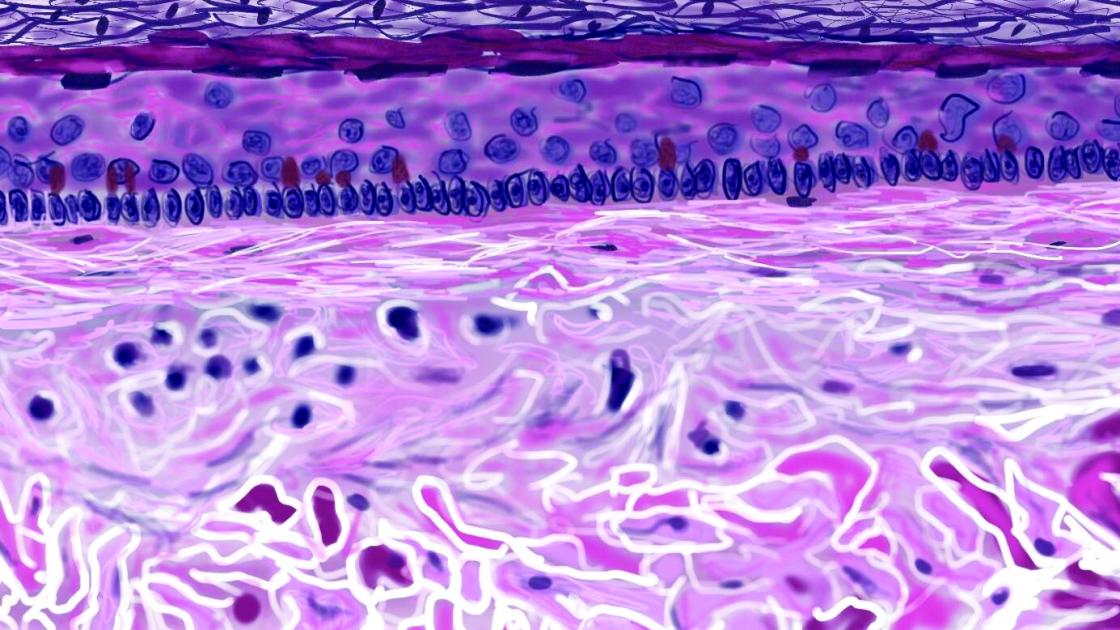
Regenerative medicine is a field that promotes creative thinking and pioneering lab engagement. “But it is not just about creating new tissue. It is manipulating cells to heal themselves,” Dr. Neumeister says. The science has been revolutionized by adding the patient’s own stem cells into the formula. Adipose stem cells derived from fat or epithelial (skin) stem cells can be combined with a specific mixture of supplements to create various tissues: skin, nerves, bone or cartilage.
“We can take a biopsy of skin from the patient, take it to the lab, dissolve it down to individual cells and then grow up a confluent sheet of skin to replace skin that’s missing, for instance, to help recovery from severe burns,” he says.
The FDA has regulations about taking the cells out of a person’s body, manipulating them and bringing them back, but a few companies are licensed to do it for specific purposes.
Two of the lab’s current projects involve using proven methods to improve surgical outcomes: cold plasma technology to sterilize skin wound areas, and the creation of a tissue “tower” containing multiple structural layers. The tower can replace a deeper injured area of a patient’s wound, from the outer epidermis down to the bone.
BONE SCAFFOLDING
An earlier study proved Dr. Neumeister’s team could grow osteoid, the foundation for bone, and integrate blood vessels that would provide circulation. But the constructs lacked the normal physiological properties that give bone its regenerative strength.
His new research entails a several-step process, beginning with bone development. A collaboration with orthopedic resident Austin Beason, MD, and plastic surgery resident Danielle Olla, MD, will use stem cells, coaxing them into bone. When combined with medical-grade glue and a blood vessel inside a tube, the cells form bone tissue. The vessel delivers nutrients to the growing cells and removes the waste.
Dr. Beason is using scaffolds as an osteoconductive matrix for the stem cells to adhere to and develop into bone.
What does a bone scaffold look like?
“It’s small; it’s a little ladder that fits in a petri dish,” Dr. Beason says. The adipose-derived, spongy material can then be customized to span the bone defect.
The next step for these experiments: giving the scaffolds a reliable blood supply and adding cartilage. Drs. Neumeister and Olla will engineer the process using microsurgical techniques. The group has grant funding for a proof of concept study to pursue the work in an animal model.

COLD PLASMA
A site visit to Carbondale 20 years ago sparked Dr. Neumeister’s interest in cold plasma. In this context, “plasma” is not referring to the yellowish component in blood. Rather, it’s the substance that is all around us, similar to a gas but with an electrical charge that causes it to behave differently through electrical interactions. Cold plasma is non-thermal. A machine bombards electrodes with argon, creating a blue flame that is warm to the touch, around 97 degrees, but doesn’t burn the skin.
With the downstate research collaboration, Neumeister proved that cold plasma was able to sterilize exposed meat, giving it an anti-microbial benefit. The finding would have numerous applications in a hospital setting. It could aid patients with large burns and protect against MRSA, the antibiotic-resistant infections that are sometimes present in medical environments.
At the time of the experiments, the cold plasma machine took up most of the room in a Carbondale lab. Today, the same result is achieved from a device slightly larger than a rolling suitcase. An even smaller model resembles a hand-held pen. Cold plasma use is prevalent in Europe, but has yet to receive FDA approval in the United States.
Jim Bruce, MD, a fourth-year plastic surgery resident, is eager to change that. Working with Neumeister and Dr. Brian Mailey, Bruce is conducting corroborating studies on the benefits of cold plasma as a sterilizing method.
Burn infections are difficult to treat and a common cause of death in burn patients. “The bacteria that infect burns are notorious for rapid development of antibiotic resistance,” says Dr. Bruce. “One of the advantages of cold plasma is that bacteria and fungus can’t become resistant to it.”
Dr. Bruce’s interest in burn recovery dates back to high school, when he was a burn patient at Loyola Medical Center in Chicago. While there, he contracted a serious infection that prolonged his course of treatment. But it also inspired his interest in a career in cellular biology and medicine. While pursuing his doctorate at Loyola University, he was able to assist on research with the physician who had treated his burn.
The regenerative medicine lab’s cold plasma machine has been used in Europe for treating diabetic foot ulcers and chronically infected wounds. Bruce, Mailey and Neumeister will repeat and expand upon studies that have shown efficacy overseas, publish their results and move it another step closer to wider acceptance. “It would be amazing to be a part of the FDA approval for this,” Bruce says.
Designing and executing these projects on a small, controlled scale in the lab provides confidence in the proof of a model. With each success in the layers of research and development, a belief is strengthened: If it can be done here, it can be streamlined and reproduced within the medical community. It is not just feasible; it can be made clinically available to patients in the very near future.



