Aortoiliac Occlusive Disease
Overview
The aorta and iliac arteries are the blood vessels in the abdomen through which nutrient-rich blood that flows to the legs must pass. Aortoiliac occlusive disease occurs when these arteries become narrowed or blocked by atherosclerotic plaque (hardening of the arteries), which is largely made of cholesterol. Aortoiliac disease is considered a type of peripheral arterial disease because it affects arteries, which are vessels that carry blood from your heart to your limbs. When your iliac arteries narrow or become blocked, your legs may not receive the blood and oxygen they need. This lack of oxygen is called ischemia and causes pain. In severe cases, sores or gangrene can develop, which can result in losing a limb. However, these developments are uncommon unless it is not treated and is allowed to progress.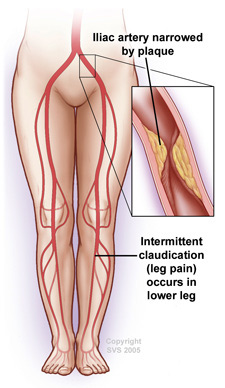
What are the symptoms?
Early in the disease, you may feel pain, cramping, or fatigue in your legs when you walk or exercise. The pain with walking usually occurs in your buttocks, thighs, and legs and goes away if you stop walking. As the disease worsens, you may find that pain occurs when you walk for shorter distances. Ultimately, as the disease progresses, you may feel pain, usually in your toes or feet, even when you are resting, and may develop sores that won’t heal, or gangrene, which may require amputation. Some men with aortoiliac occlusive disease also experience erectile dysfunction, the inability to have or maintain an erection.
What causes aortoiliac occlusive disease?
Atherosclerosis, or hardening of the arteries, causes most cases of aortoiliac occlusive disease and is related to smoking, high cholesterol levels in the blood, high blood pressure, obesity, and having a family history of heart disease.
What can I expect?
First, your physician will ask you questions about your general health, medical history, and symptoms and will perform a physical exam. Your physician will want to know when your symptoms occur. If your physician suspects you may have aortoiliac disease, he or she may perform tests to further define its severity, such as measuring the blood pressure in your arms, ankles, and toes. Your physician may also use an ultrasound to try to locate the exact area of blockage. If your symptoms are severe enough to warrant treatment your vascular surgeon will perform angiography to obtain more precise information about the location and severity of your blockages to better guide your treatment.
Angiography
There are three types of angiography: contrast arteriography, CT angiography (CTA), and MR Angiography (MRA). Contrast arteriography usually provides better resolution but is a more invasive test. Your physician injects a contrast dye into your arteries and then takes x-ray images. This test finds the exact location and pattern of blockages. The dye is excreted from your body through your kidneys. If a blockage is identified and is appropriate for treatment by angioplasty and stenting, this procedure may be carried out at the same time. CTA and MRA are alternative less invasive methods to look for blockages, but do not provide the same quality of imaging or the opportunity to treat with angioplasty and stenting.
How is aortoiliac occlusive disease treated?
Lifestyle Changes
In mild to moderate cases, your physician may recommend that you change certain aspects of your lifestyle like quitting smoking, maintain a healthy weight, following a structured walking program at least 3 or 4 times a week, and eating a low-fat and high-fiber diet. If necessary, your physician may prescribe medications to lower high cholesterol. If you have diabetes, you need to control your blood sugar levels with diet and medication.
Medications
If you do not have a disqualifying medical condition, such as heart failure, your physician may also prescribe cilostazol (Pletal), which may improve the distance you are able to walk without pain, or aspirin or clopidogrel (Plavix), either of which can lower your chances of blood clots. Statins are a class of medications that your physician may use to control your cholesterol levels. None of these medications will “cure” you of the disease, but are important at relieving some of your symptoms, and may help protect your arteries from developing further disease.
Angioplasty or Surgery
If you have severe aortoiliac occlusive disease, particularly if it does not improve with the measures described above, your physician may recommend a minimally invasive treatment called angioplasty to improve the circulation in your legs. For more extensive blockages or those that cannot be treated with angioplasty, surgery to clear your blocked arteries may be required. During an angioplasty procedure, which is sometimes performed at the same time as an angiogram, a balloon is inflated within the blocked area to stretch the artery open. In some circumstances, a tiny mesh-metal tube called a stent may then be placed into the narrowed area of your artery to help keep it open. The stent remains permanently in your artery. After successful angioplasty, blood flows more freely through your artery. Bypass surgery, usually performed through abdominal or leg incisions depending upon the location of the blockage, creates a detour around the narrowed or blocked sections of your artery. A synthetic fabric tube (often Y shaped) called a bypass graft is attached to your aorta above the blockage, with the other end being attached to the leg artery or arteries downstream of the blockage. Although more invasive than angioplasty, bypass surgery restores blood flow in over 90% of patients and typically lasts longer than angioplasty, with results commonly being maintained for 10 or more years. An endarterectomy, which also requires incisions to expose the arteries, is a way for your surgeon to remove the plaque from your artery, leaving a wide-open artery and restoring blood flow to your leg. The best choice of the treatment options depends upon the pattern of blockage as well as how much blockage you have. Your vascular surgeon will help you determine which method of treatment is best for your particular situation.
Why SIU
Continually learning
With a focus on continual improvement, our doctors take the time to research, study and innovate to provide the latest treatments for our patients.
Patient-first experience
Our care ranges from primary care physicians to specialists and sub-specialists who have advanced training. We're here for you when you need us.
Breakthrough tech
Continually teaching the next generation of doctors, our physicians use the latest developments in procedures and technologies for our patients.
